Date: Friday, April 12th | Felix Serratosa room | 12|04|2024 Time: 10:00 AM Speaker: Valerio Di Domenico Guerin…
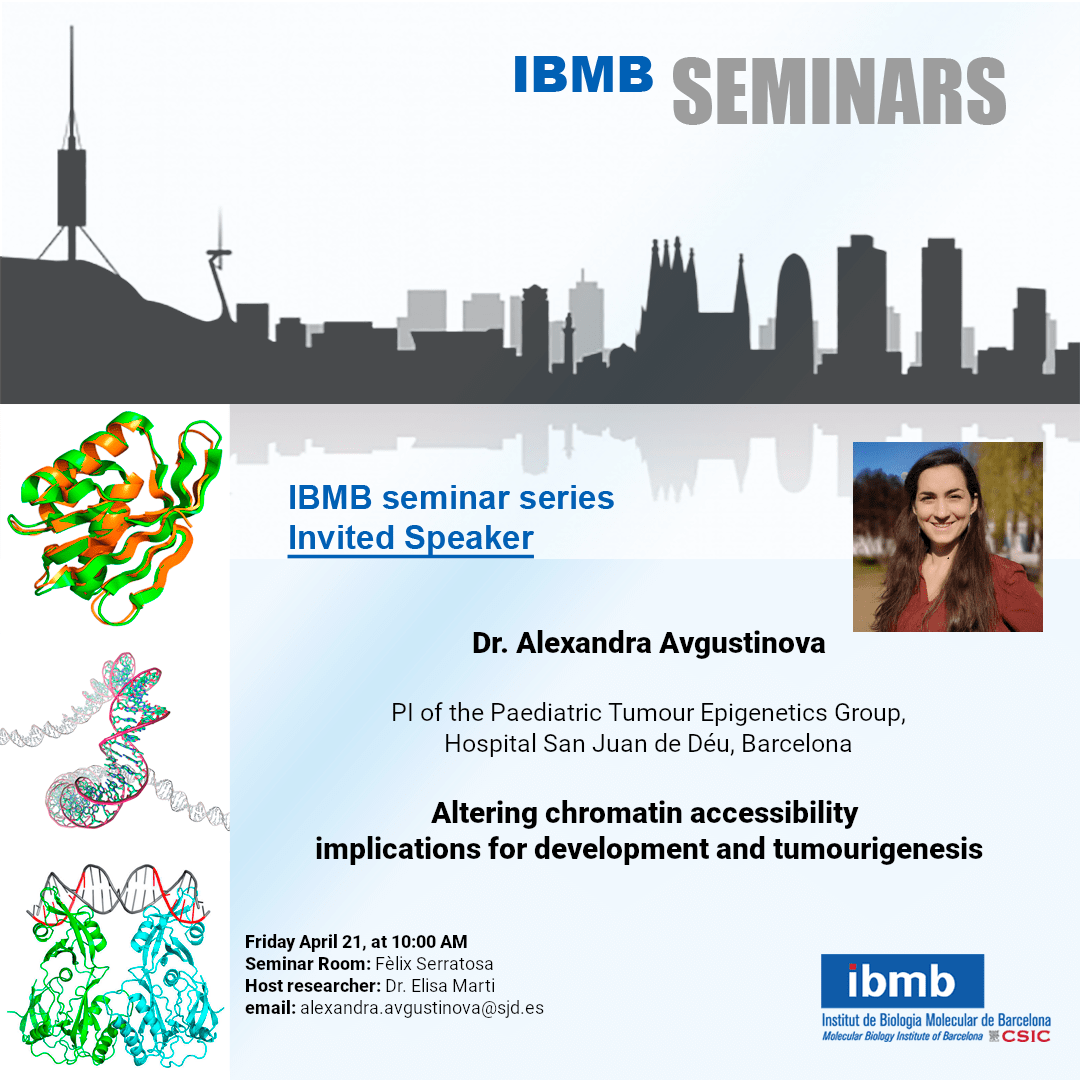
IBMB Seminar, Friday, Apil 21th 10:00 AM | DR. ALEXANDRA AVGUSTINOVA
Date: Friday, April 21th | Felix Serratosa room | 21|04|2023
Time: 10:00 AM
Speaker: Alexandra Avgustinova.
Paediatric Tumour Epigenetics Group
Title: “Altering chromatin accessibility – implications for development and tumourigenesis“
Email: alexandra.avgustinova@sjd.es
Host researcher: Dr. Elisa Marti
Seminar Room: Fèlix Serratosa
Abstract:
Nearly 25% of all cancers harbour mutations in constituents of the SWI/SNF chromatin remodelling complexes, indicating a potentially functional role of chromatin accessibility dysregulation in oncogenic transformation. Indeed, biallelic inactivation of the SWI/SNF subunit SMARCB1 is a hallmark feature (>95% penetrance) of malignant rhabdoid tumours (MRTs), and constitutes (together with SMARCA4, to a much lesser extent) the only recurrent mutation in these tumours. MRTs are remarkably genomically simple tumours: chromosomal aberrations are rare, and their genomic mutation rate is among the lowest of any cancer. Hence, SMARCB1-loss in MRTs is the purest known instance of epigenetically-driven oncogenic transformation. MRTs are usually diagnosed in infants <2 years of age and prognosis is abysmal due to fast tumour growth, local invasiveness and metastasis, with 5-year survival of <20%. Current treatment strategies involve a multimodal regimen combining tumour resection, radiotherapy and chemotherapy, which have grave long-term side effect when employed in children.
Therefore, there is an urgent need to understand the mechanisms of epigenetically-driven malignant transformation to allow for the pursuit of more personalised and less toxic and mutagenic approaches to MRT treatment. Important outstanding questions include: What is the cell-of-origin of MRTs? How does epigenetic reprogramming in this cell-of-origin cause malignant transformation? Can we reverse these epigenomic alterations to trigger terminal differentiation of MRTs? Can we exploit epigenomic dysregulation to enhance the immunogenicity of MRTs and hence the utility of immunotherapy in their treatment?
We study these questions using three complementary approaches: (1) a well-characterised cohort of 20 patient MRTs; (2) a tightly controlled patient-derived isogenic experimental system of SMARCB1 re-expression, and (3) patient-derived and transgenic MRT mouse models.
The use of these three approaches in parallel allows us to experimentally identify molecular pathways of epigenetically-driven oncogenic transformation while at the same time testing the relevance of the findings on real-life patient tumours. Ultimately, based on the epigenomic understanding of the tumours, we aim to unearth new intervention nodes for the treatment of MRT cancer patients.